Have you noticed a little change on nutrition labels? Vitamin A used to be listed in IU’s (International Units), but is being changed to µg RAE (Retinol Activity Equivalents).
Apparently Vitamin A is more complex than initially thought. There’s so much more to it than eating carrots for good eyesight! Vitamin A is still fat soluble. It’s still important for vision. It is also critical for things like immune function and modulating inflammation – especially important if you have an autoimmune disease! What’s changed is what we know about how Vitamin A is metabolized.
- animal sources contain pre-formed Vitamin A (retinol & retinyl ester)
- plant sources contain many different kinds of pro-vitamin A carotenoids, including but not limited to:
- alpha-carotene
- beta-carotene
- beta-cryptoxanthin
Our bodies bio-convert all of these nutrients so that we can use the active form of Vitamin A: retinal (and retinoic acid). It turns out that what researchers have learned about this process led to the change in units from IU to RAE. There’s a difference in how nutrients convert depending on their source. Confounding the researchers, when looking at IU’s, foods supposedly containing the same amount of Vitamin A can metabolize to vastly different amounts of usable retinal, which means that there isn’t a simple conversion factor to use to change all IU’s to RAE’s.1 Although we absorb about 70-90 percent of pre-formed vitamin A from animal sources, carotenoids are a different story. Plant-based Vitamin A is not metabolized nearly as well.
Consider two foods that many people consider disgusting: kale and liver. Both are good sources of Vitamin A, yet the nutrients look quite different between the old and new units of measure.
| Kale (1 C = 67 g) | 10,302 IU | 515 mcg RAE |
| Beef Liver (2 oz) | 9,600 IU | 2,805 mcg RAE |
IU’s make it look like kale has more Vitamin A, but when we look at how much retinal our bodies get to use from these foods, a serving of liver has more than five times as much.
Vitamin A & Autoimmunity
For years, some people have suggested that autoimmune diseases are caused by nutrient deficiencies. Nutrition is especially important to people with autoimmune diseases. In the case of Vitamin A, we need sufficient amounts for our bodies to work correctly. Unfortunately, sometimes people think that they can just take a handful of vitamin pills instead of eating properly. It doesn’t work that way. We need to consume plenty of Vitamin A-rich foods if we’re to be as healthy as possible. Vitamin A is needed to do many things, including:
- form natural killer cells
- increase phagocytes to fight infection
- increase anti-inflammatory cytokines
Why the Change in Units?
The newer research about how bioconversion takes place indicates that some people are not getting nearly as much Vitamin A as they thought since not all IU’s are metabolized the same. Switching to RAE’s is better because it gives us a more accurate picture of the nutrients our bodies actually get to use.
One cup of kale provides 74% of the Recommended Daily Allowance for Vitamin A, while a two ounce serving of liver (because, honestly, who can stand to eat much more than that?) is well over the RDA and nearly to the tolerable upper limit (UL).
Yep, there’s an upper limit. Just as it is important to get enough Vitamin A, it is also important not to get too much. Toxicity can result from excessive intake. Vitamin A toxicity is more common when people are taking supplements, but can happen through dietary intake, too, generally from excessive amounts of liver. I find it slightly ironic that eating too much liver can be harmful to our livers.
Symptoms of toxicity are numerous and can include headaches, dizziness, nausea, joint pain, peeling skin, and in extreme cases coma, or even death. Severity depends on how much Vitamin A was ingested, and how fast. This theory says that symptoms would be more severe for a person who eats 5,000 mcg in one sitting, compared to a person who eats 1,100 mcg three times a day. Am I a terrible person for thinking that anyone who eats 4 ounces of liver shouldn’t be surprised that it makes them sick?
Curiously, excess plant-based Vitamin A is not toxic. The most-reported symptom is orange skin. I know someone whose baby loved carrots and ate so many that his face turned orange. Skin returns to its normal color when plant-sourced Vitamin A consumption is reduced.
So how much is enough, and how much is too much?
According to the current research, dietary needs increase as we grow. Adult men tend to need more than adult women (probably because they tend to have larger bodies).

Do you ever wonder if people are just throwing darts at a dart board in making these recommendations? At least 700 µg RAE every day?! Are they out of their ever-lovin’ minds? People would have to quit their jobs and spend all their time menu planning & cooking in order to find a way to get that much Vitamin A on a regular basis!
How Do We Get Vitamin A?
We can get some Vitamin A from plants. The best plant sources are bright orange or leafy green. Carrots and sweet potatoes (but not yams) have the most, followed by foods like kale, turnip greens, dandelion greens, radish leaves, and cantaloupe.
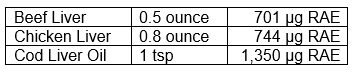
However, the Vitamin A from plants is in the carotenoid forms and isn’t metabolized very efficiently. We’re supposed to get animal sources, too. If you don’t consume dairy or eggs (which is now recommended by many), that means liver. Beef liver. Chicken liver. Liverwurst. Foie Gras. Braunschweiger. Cod liver oil. Liver is an excellent source of Vitamin A.
Don’t eat too much, because toxicity – mentioned previously – is a real thing. One source recommends limiting liver to six ounces per week, maximum.
From a Vitamin A standpoint, it’s not even necessary to eat that much liver. We could actually get our entire RDA of Vitamin A by eating half an ounce of beef liver daily. Or bring back the practice of taking a daily spoonful of cod liver oil.
But don’t get stuck in a rut. We’re actually supposed to get our nutrients from a variety of sources instead of eating the same thing every day. The USDA’s FoodData Central website has nutrient information on pork liver, veal liver, lamb liver, turkey liver, goose liver, duck liver, sea lion liver, walrus liver, and even moose liver — but not elk or deer, which are livers that I actually have access to. Go figure. Anyhow, what it comes down to is that unless you’re eating a ton of vegetables, you should probably eat liver, but a little bit goes a long way.
If you’re curious about the actual amounts of Vitamin A in veggies:


By comparison, other veggies don’t have nearly as much Vitamin A2. They do, however, contain other nutrients, so don’t neglect them:




So there you have it. Switching the units from International Units to Retinol Activity Equivalents lets us look at nutrient information and know how much Vitamin A our bodies will actually be able to use.
* * * * * *
For Further Reading:
- Vitamin A (NIH)
- Vitamin A (Medline Plus)
- Vitamin A Fact Sheet for Health Professionals
- The Telltale Liver
- The Perils of Eating Polar Bear
- Hypervitaminosis A
___
1Converting from IU’s to RAE’s:
- For meat and eggs (retinol sources), multiply IU by 0.3 to find mcg RAE
- For fruits and vegetables with beta-carotene, multiply IU by 0.05 to find mcg RAE
- For fruits and vegetables with alpha-carotene or beta-cryptoxanthin, multiply by 0.025 to find mcg RAE
2Nutrient info is from the US Department of Agriculture’s FoodData Central website, glycemic load information is from Self’s NutritionData database. Color groups shown are based on Dr. Terry Wahls‘ research, wherein she recommends eating 3C of leafy greens, 3C of brightly colored (try to hit more than one color), and 3C sulfur-rich foods daily. I have omitted nightshades and legumes because they are disallowed in the elimination portion of Wahls and AIP. Legumes didn’t make the re-intro cut for me (not a problem since I’m allergic to soy and probably peas and peanuts), and the only nightshade I really do okay with is tomatoes if they’re organic (but I react to standard store-bought tomatoes). More than you ever wanted to know, but that’s what determined what’s on the lists.






